Tulane wins $2.27 million grant to combat burnout among health care workers
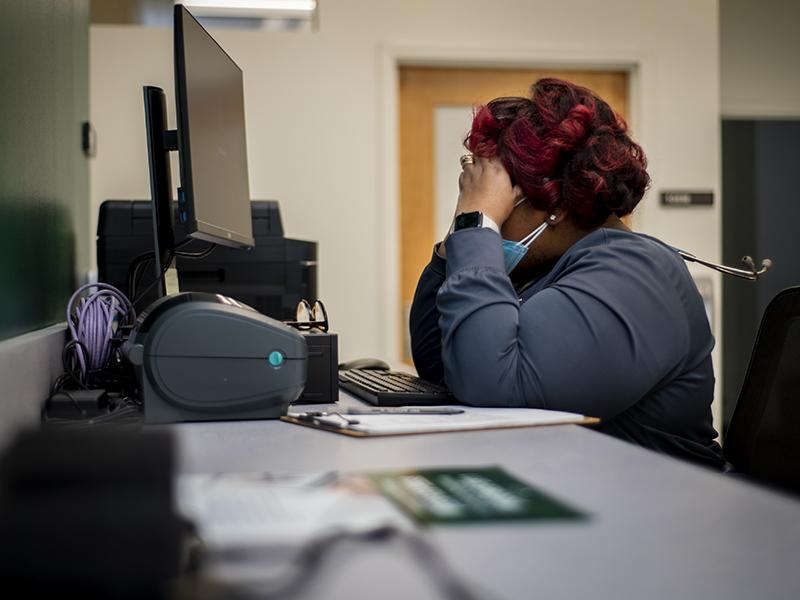
Health care workers experience alarming levels of burnout, low job satisfaction and compassion fatigue, leading to poor behavioral health outcomes for themselves and contributing to increased health disparities for the communities they serve.
The Tulane University School of Social Work (TSSW) plans to address these issues as part of a $2.27 million grant from the U.S. Health Resources and Services Administration.
Over the next three years, TSSW will team up with Access Health Louisiana, a network of community health clinics, to develop, implement and disseminate innovative, evidence-based self-care models that address retention, burnout and overall wellbeing and resiliency of the health care workforce.
The program is called Project RETAIN (Resilient, Empowered, Trained and Invested Network). Initially, it will target health care workers in rural, medically underserved communities in the Gulf South, with longer-term goals of taking the program regionally and nationally.
"Tulane School of Social Work has well-regarded experts who have significantly contributed to the knowledge base around burnout, compassion fatigue and resilience,” said TSSW Dean Patrick Bordnick. “This grant enables us to apply this expertise to assisting the helping professions in the here and now so that they can better care for the broader community and fill the emerging needs to come."
The study will be led by Tonya Hansel, PhD, director of TSSW’s doctorate program, and include numerous faculty members. Others on the team include Anneliese Singh, Tulane’s chief diversity officer and a TSSW faculty member; Stephen Murphy, an assistant professor in Tulane School of Public Health and Tropical Medicine; and experts from Access Health Louisiana.
"Workforce retention and healthcare provider shortages are concerning, and an increase in current deficits is estimated through 2030,” Hansel said. “The COVID-19 pandemic made many existing burnout prevention and job satisfaction efforts challenging. The pandemic caused people to work even longer hours in high stress situations increasing pre-existing burnout.
“We need to understand how chronic slow burn stressors impact these workers’ lives,” she said. “There’s so much more about what we don’t know that can support those in these fields stay committed in a healthy way.”
Project RETAIN will employ a multi-component, evidence-driven strategy to achieve its goals. It will begin with a series of surveys and interviews with health care workers and agencies to reduce gaps in knowledge regarding self-care needs and barriers. Based on those responses, the team will implement short-term resilience trainings to foster compassion fatigue resilience and reduce burnout.
Health care workers will participate in three self-care service models – routine self-care training, or standard care; innovative engagement in activities selected by health care workers; and access to virtual reality mindfulness approaches.
“Evaluation of these approaches will increase understanding of how well and for whom different approaches work,” Hansel said. “This information is critical to the development of sustainable, cost-efficient interventions that can be tailored to a diverse, multi-setting healthcare workforce.”
Based on ongoing evaluations, the team will develop and implement a training-the-trainer toolkit aimed at expanding the reach of the program to approximately 6,500 health care workers.
“Everyone will benefit,” Hansel said. “People will have access to help when they need it, and services improve when those who stay in the profession longer can become better trainers and mentors to those newer to the profession.”