Is the nose key to preventing pneumonia? Tulane awarded $7.5 million grant to investigate
Tulane University has been awarded a seven-year, $7.5 million grant from the National Heart, Lung, and Blood Institute to study how boosting immune cells in the nose could lead to stronger, longer-lasting protection against pneumonia — the world’s leading infectious killer of children.
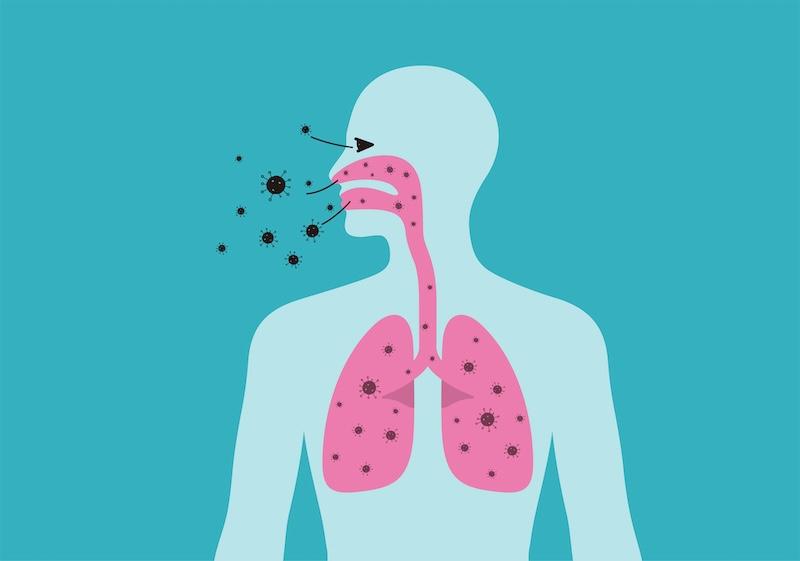
Pneumonia is an infection in the lungs caused by bacteria, fungi or viruses. While current vaccines offer protection, they don’t cover all strains of pneumonia, creating a “whack-a-mole” approach that can leave some vulnerable to infection.
The study, led by Dr. Jay Kolls, director of the Center for Translational Research in Infection and Inflammation at Tulane University School of Medicine, will focus on a group of immune cells called CD4+ T cells which serve as frontline defenders for the respiratory system. Kolls believes a subgroup of these cells in the nose can be harnessed to boost pneumonia prevention.
“A lot of people don’t realize it, but bacterial pneumonia is preceded by initial bacteria colonization in the nose,” Kolls said. “Theoretically, the longer the bacteria stay in the nose, the higher the risk of developing pneumonia in the lungs. If we can understand what keeps these immune CD4+ T cells alive and functional, this may result in longer-lasting and broader immune protection against pneumonia.”
Prior research showed CD4+ T immune cells to be pivotal in combating pneumonia. Kolls and his team will be studying a subgroup of these immune cells in the mucosal lining of the nose and lung that produce IL-17, a molecule critical for protection against bacterial and fungal infections. Additionally, immune cells that survive encounters with pathogens can become memory cells, which are able to more rapidly identify and respond to future threats from disease.
To shed light on the function and lifespan of these cells, Kolls’ lab will use single-cell sequencing techniques to create an atlas of T cell receptors throughout the respiratory system from the nose to the lung.
“If you don’t have IL-17 in your nasal passages, you don’t clear the bacteria,” Kolls said. “We know it’s important. What we don’t know is how long these T cells and memory cells last and what we can do to ensure their longevity.”
While current vaccines may only work against approximately 20 of the more than 100 strains of the leading cause of bacterial pneumonia, T cells can recognize proteins shared across bacterial strains, potentially providing the foundation for more robust vaccines or immunotherapy that can offer broader immunity.
Pneumonia poses a severe threat to infants and children, whose immune systems are still developing. However, adults are still at risk. Pneumonia remains a leading cause of death among adults in the U.S., killing approximately 50,000 a year. Kolls has witnessed firsthand the rise in pneumonia cases among those with HIV, which attacks and destroys key immune system defenses.
“We think controlling the nasal microbiome can regulate our susceptibility to infection,” Kolls said. “By furthering our understanding of the mucosal immune system, we hope to improve strategies for reducing pneumonia incidence and prevalence.”