Tulane researchers awarded Fast Grant for second-generation COVID-19 vaccine
As pharmaceutical firms race to bring the first COVID-19 vaccines to market, scientists are already working on version 2.0. Two Tulane University researchers were awarded a $150,000 Fast Grant for a project to make next-generation COVID-19 vaccines more effective.
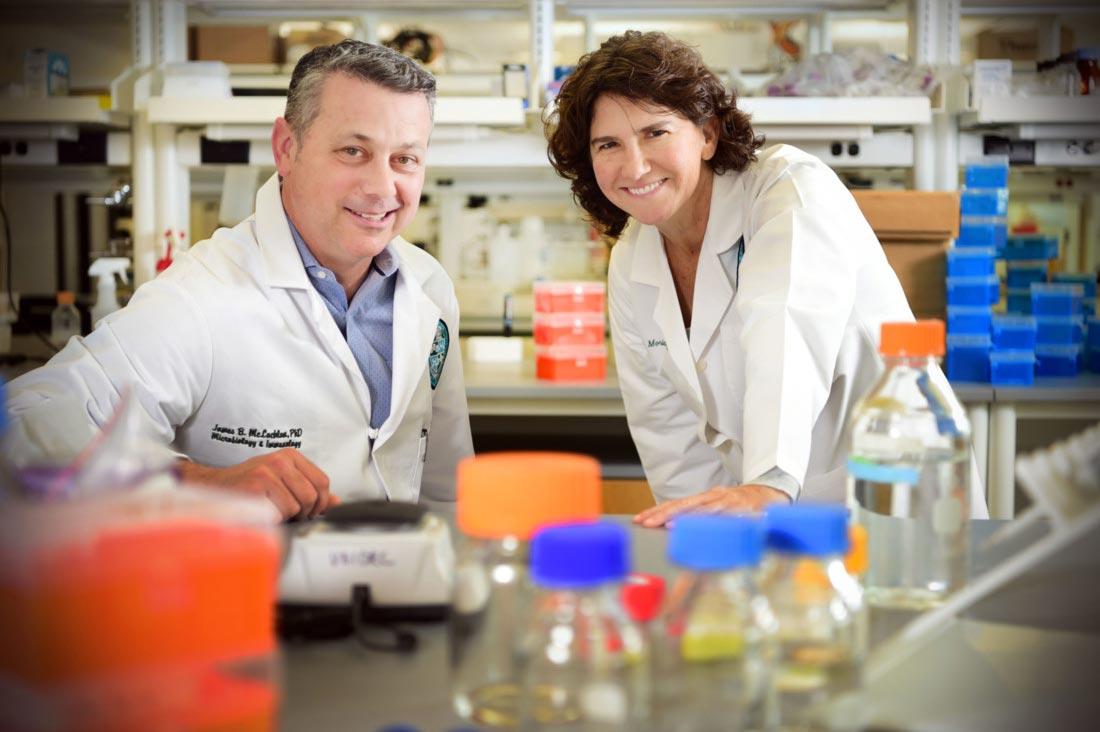
Microbiologist Lisa Morici, PhD, and immunologist James McLachlan, PhD, will test whether they can elicit a better immune response in tissues most vulnerable to SARS-CoV-2 infection — the lungs and gut — by adding two bacteria-based adjuvants to COVID-19 vaccines in development. Adjuvants are ingredients used in vaccines to trigger an immune response.
“Despite the rapid deployment of vaccines for SARS CoV-2, there is considerable uncertainty whether first-generation vaccines will halt the pandemic,” said Morici, associate professor of microbiology at Tulane University School of Medicine. “Vaccine adjuvants have the potential to dramatically improve the overall vaccine efficacy, and adjuvant choice is critical for driving the desired type of immune response.”
The current top vaccine candidates use parts of the virus to trigger the body to produce antibodies, B cells and T cells. It’s unclear how long these immune responses will last and whether people will need multiple doses of the vaccine for long-term protection.
The researchers will study two vaccine adjuvants: a modified toxin derived from E. coli called dmLT and another based on outer membrane vesicles (OMVs), which are nanoparticles shed by bacteria. Both adjuvants were developed at Tulane through support from the NIH Adjuvant Development Program. Morici and McLachlan have shown in previously published work that their adjuvants can stimulate the production of antibody-producing B cells and virus-fighting T cells in the tissues of the lung and gut.
“We're using adjuvants to actually drive these immune responses to the tissues where they're needed most,” Morici said. “If we can use our adjuvants to induce antibodies as well as tissue-resident B and T cells, we can provide a much longer window of immunity in the very tissues where that immunity is most effective. The scientific evidence also suggests that tissue-resident immune cells may last longer than those in the blood.”
Researchers will study the adjuvants in combination using a mouse model of COVID-19. They will look at the different ways the immune system responds to vaccination as well as their overall protective abilities when the mice are challenged with the virus.
Fast Grants are funded through the Mercatus Center at George Mason University. They are unusual in their speed as they are awarded within 48 hours of application to get funding to researchers as quickly as possible. The program is modeled after the work of the National Defense Research Committee, an organization which provided quick funding for scientific discoveries and technological developments in World War II.