Tulane professor receives NIH supplement for Alzheimer’s research
There are 5.7 million people living with Alzheimer’s disease, according to Alzheimers.org, and the dreaded disease has caused more deaths than both breast and prostate cancer combined. Finding a cure is paramount.
Andrea Zsombok, an associate professor of physiology in the Tulane University School of Medicine and member of the Tulane Brain Institute Executive Committee, recently received a $334,000 supplement to her current National Institutes of Health (NIH) grant that supports research into the brain’s role in diabetes. Diabetes is associated with an increased risk for all dementias, including Alzheimer’s disease.
Zsombok, whose research is mainly associated with the Brain Institute’s brain-body health research cluster, initially received a $1.6 million grant from the NIH in 2014. The additional grant will supplement studies that are extensions of the original award. The goal of these studies is identifying the activity of liver-specific neurons in a model of Alzheimer’s disease.
“The knowledge gained from the studies may lead to new strategies to improve glucose homeostasis before the full development of Alzheimer’s disease as well as a better understanding of how disruption of the central control of glucose homeostasis exacerbates the disease pathology,” Zsombok said.
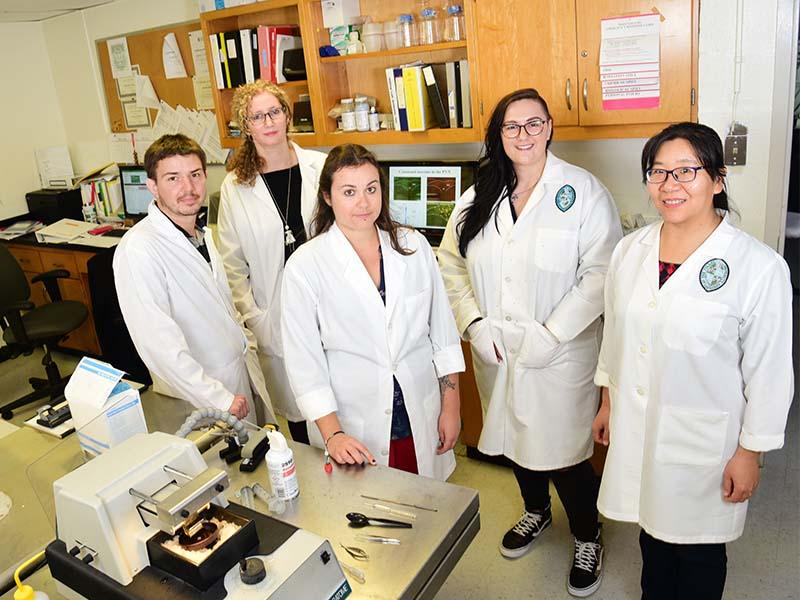
Zsombok and her team members – postdoctoral fellows Lucie Desmoulins, Hong Gao and Adrien Molinas, along with graduate student Sierra Butcher and medical student Cassidy Werner – are studying the autonomic nervous system, which mainly acts unconsciously and regulates bodily function. It also contributes to the regulation of systemic sugar levels. Research has suggested there is a high risk of developing diabetes if autonomic dysfunction is present.
Therefore, without a full understanding of the mechanisms controlling the brain-liver pathway, which is essential for the maintenance of glucose levels, there is a barrier to understand the brain control of sugar levels.
The overall goals of the initial award are to identify neurons, which are part of the brain-liver pathway, investigate their activity in healthy and diabetic conditions, and determine the reason for their dysfunction during diabetes.
“Our publication shows that in a diabetic condition the neurons, which are part of the brain-liver pathway, are more active than in a normal condition. So, likely there are differences in the brain of a person with diabetes compared to a healthy person in a context of the brain-liver pathway,” Zsombok said.
Zsombok described this process similar to when an individual endures stress, such as being scared. The body activates the sympathetic nervous system (SNS), which leads to a cascade of responses, including the release of glucose. This process would provide a healthy individual enough energy to deal with the situation. Unfortunately, in many conditions like diabetes or hypertension, these individuals have already reached a higher activity of the SNS, which contributes to the higher sugar levels. One of the goals of Zsombok’s research is to find a way to decrease this activity that could be beneficial for regulating glucose.
The Tulane Office of Research established in the Brain Institute an interdisciplinary working group on Alzheimer’s disease and cognitive aging, including funds invested through the Brain Institute to support the growth of research in this critical area.